The Role of Public Health Data Management on the Rising Monkeypox Numbers
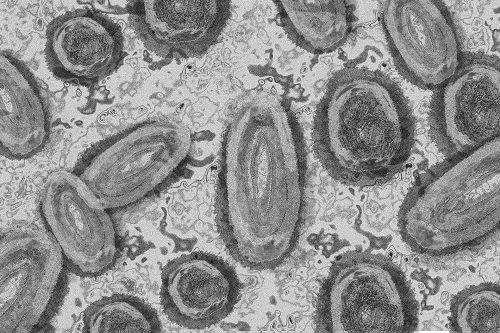
It has been over three months since the first case of monkeypox was reported in the United States, but access to quality public health data remains limited across the country. There are now over 15,000 reported monkeypox cases in the U.S., and the infection rate continues to accelerate dramatically. Public health agencies at the federal, state, and local levels are working to coordinate their response efforts, but many agencies have yet to share their data with the Centers for Disease Control and Prevention (CDC). When the agency updated its infection rate in late July, it had only detailed about half the reported cases, according to CDC Director Rochelle Walensky.
The pace and scope of the outbreak have caught many countries and public health agencies by surprise, even after the COVID-19 pandemic instilled the need for public health data interoperability and disease response preparedness. But pandemics are random by nature, and there is no telling when the next one will strike.
Monkeypox is now a reportable disease. A state-run immunization information system (IIS) can now work with private healthcare providers to collect data on the number of people who have received the smallpox vaccine. An electronic disease surveillance system (EDSS) can collect data on the number of people that have been infected with the virus. But these systems must share their data with each other and public health agencies at all levels of the government to contain the outbreak.
However, states are not required by law to share this information with the CDC. They can do so on a voluntary basis. When asked about their ability to share public health data with the government, 29 states responded and said they were committed to sharing their data with the CDC. But many were still in the process of collecting information about the virus and the vaccine.
Access to public health data is essential when responding to a pandemic. In the case of monkeypox, public health officials are still trying to determine which groups of people are most likely to be infected and how the virus spreads. Identifying the group with the highest risk allows providers to focus and target their messaging to help members of the public protect themselves from infection.
Improving the quality of the data the EDSS receives will give providers and public health officials more information about who is most at risk. The infection data should include information about the person’s sexual preferences, their sexual history, and with which gender they identify, so healthcare officials and providers can focus on informing individuals in this group of their risk of infection through public messaging.
However, the input fields on the EDSS may prevent providers from including this information. For example, the gender identification form may only include a male and female option without leaving space for nuance, including transgender men and women and those identifying as non-binary. The sexual preference field may classify a person as homosexual or heterosexual without taking into consideration bisexuality or the person’s complete sexual history. The number of sexual partners can also come into play, but many disease surveillance systems do not let providers specify the number of sexual providers.
Public health data can also give healthcare providers and public health agencies insight into the efficacy of the monkeypox vaccine. It is the same vaccine used for the smallpox virus, which is related to the monkeypox virus. Still, there has yet to be a clinical trial documenting its ability to block infection. Public health agencies need to be able to cross-reference the IIS data with that of the EDSS to understand how well the vaccine is working. This shows whether those that have received the vaccine are vulnerable to infection.
Time is always of the essence when responding to an infectious disease outbreak. The number of reported monkeypox cases continues to rise exponentially, and many organizations struggle to keep pace. Data interoperability is key to overcoming these challenges. Public health workers and private providers must be able to quickly organize and share their findings. Convenience and ease of use will increase participation in the data sharing program. The software should be able to incorporate various types of data from a range of different sources into a single database. Many states have set aside funding to update public health data management, which will improve the way providers and officials collect and share this information.
Access to quality, robust data also gives public health officials the resources to anticipate future trends in the pandemic. Doctors and officials will be better prepared to direct funding if the situation escalates. Officials can also use this data to advise President Biden on whether he should declare a state of emergency, which would increase urgency and give states more resources to combat the outbreak. Infection and vaccination information is essential in the fight against monkeypox. Using the right technology can improve the reporting and data management process.
As we confront the challenge of rising monkeypox numbers, the significance of robust our disease surveillance solutions cannot be overstated. These solutions empower public health officials with the data analytics and reporting tools necessary to track outbreaks, manage cases, and deploy resources effectively. By integrating advanced data management practices, health departments can enhance their response strategies, ensuring timely interventions and informed decision-making to curb the spread of monkeypox and protect public health.